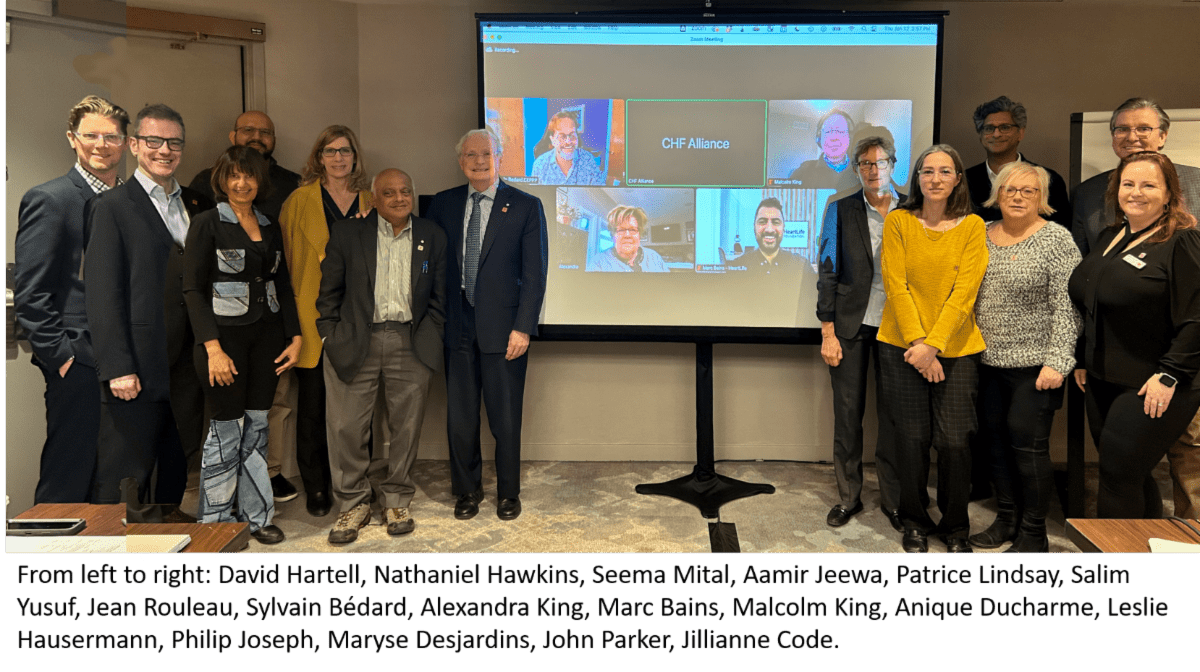
Jean Rouleau
The Canadian Heart Function Alliance (CHF Alliance) Network brings 132 Canadian researchers and clinical experts in heart failure (HF) in eight provinces and one territory, together with patients, caregivers, Indigenous Elders and Knowledge Holders, policymakers, knowledge users, not-for-profit organizations, health care providers, academic institutions, and industry partners to improve the prediction, prevention, diagnosis, and management of HF.
Led by Jean Rouleau, HF pioneer at Montreal Heart Institute, with Marc Bains, a patient living with HF and a founder of HeartLife Foundation, the CHF Alliance is patient-driven, spanning children to elderly people, rural to urban centres, and across socio-economic barriers. The CHF Alliance has already attracted matching funds of over $27 million to complement a $5 million investment from the Canadian Institutes for Health Research (CIHR) and Heart and Stroke Canada.
The CHF Alliance has 23 research projects; the projects listed here are the ones led/ co-led by PHRI researchers.
Translational science and population health

Philip Joseph
Led by PHRI’s Philip Joseph and Salim Yusuf, with E. O’Meara and C. Yip, the Translational Science Team aims to better understand the determinants of progression from risk factors to HF and to death; and test whether interventions at various stages prevents progression and improves prognosis. HF is the end result of several complex processes that are only partially understood, with differing phenotypic presentations, and a range of comorbidities that impact survival and QOL.
The theme of translational science and population health will focus on important, but relatively neglected, areas of HF research, including ageing, comorbidity, and HF, and improving delivery of HF care.
Projects will focus both on knowledge generation and on testing interventions, We will leverage big data collected through ongoing large, prospective cohorts that we have brought together, and apply advanced analytic methods to gain novel insights into determinants for HF development and progression. The population cohorts are PURE, CLSA, and CAHHM which collectively have more than 2,000 new incident HF events.
The Global-Congestive HF (G-CHF) study of 23,000 patients with HF (4000 patients have detailed measures of diet, frailty, lung function, depression, cognition; and 3000 of these have ‘omics’ data) has already recorded 5,000 deaths and 10,000 hospitalizations after 2 years follow-up: 10,000 deaths and 18,000 hospitalizations are expected in this cohort after the planned 5 years of follow-up.
We will also leverage our substantial clinical trial experience to develop a pan-Canadian HF trial network to implement pilots and full scale studies. This will include seed funding for pilot studies to be leveraged to obtain external funding for definitive trials and enhancing capacity to conduct high impact trials in HF in Canada.
Biological pathway discovery

Salim Yusuf
A team led by Guillaume Pare and Salim Yusuf will look at biological pathway discovery. Through case: control analysis of 3,000 HF cases from G-CHF and 5,700 matched controls from PURE, we will analyze 356 biomarkers (partial funding secured) associated with inflammation, immunity, oxidative stress, endothelial function, energy metabolism, myocardial injury, extracellular matrix remodeling, cellular adhesion, neuro-humoral regulation, and vascular regulation using a multiplex biomarker platform.
Significant biomarkers will be examined for causality by utilizing Mendelian randomization and will be validated with findings in external genetic HF cohorts (HERMES Consortium) and in independent databases – such as the UK Biobank, and the National Heart, Lung, and Blood Institute (NHLBI)’s HeartShare.
AI-based HF pheno-mapping
Led by Philip Joseph and R Avram, artificial intelligence and machine learning will be used to identify distinct phenotypic subsets of HF using clinical, echocardiographic and biomarker data in 23,000 people in G-CHF and in a subset of 4,000 people who have additional data on lung function, frailty, nutrition, and exercise capacity. Unsupervised machine learning will identify HF subtypes with distinct clinical and biological features both for HFpEF and for HF with reduced Ejection Fraction (HFrEF).
Collaboration with NHLBI HeartShare will permit standardized approaches to phenotyping, and cross validation of findings.13 This will inform future precision based strategies for HF treatment, particularly in HFpEF.
Predicting HF in Indigenous populations

Russell De Souza
Indigenous populations may have a unique risk factor profile for developing HF. This team, led by Sonia Anand and Russell DeSouza, will identify key traditional (e.g. diabetes) and non-traditional risk factors (e.g. air pollution, social support) for cardiac dysfunction leading to HF among 2,500 Indigenous people enrolled in two cohort studies (CAHHM First Nations cohort and CLSA) with detailed clinical and community-level risk factors, and cardiac MRIs. They will use supervised machine learning methods to identify factors associated with changes in cardiac structure and function on cardiac MRI, and with incidence HF (during follow-up) in CAHHM-FN.
Significant risk factors will then be used to develop a risk score for pre-clinical cardiac dysfunction, which can be applied to predict incident HF in CAHHM-FN, with validation among CLSA Indigenous participants (1800). In the CAHHM-FN cohort, an excellent working relationship has been developed between Indigenous and academic researchers, with a tested governance model whereby each FN community owns their own data and can choose to participate in specific analyses and publications.
An annual Indigenous data workshop of CAHHM-FN is held to share findings, interpret them, and build research capacity. This is highly valued by that community as a positive step toward self-governance in research.
Inflammation in HF
Inflammatory pathways are upregulated in some ‘cardio-inflammatory’ HF subtypes and this is associated with worse outcomes. Inhibition of inflammatory pathways (e.g. IL-1b) could improve HF related outcomes. The team will test the efficacy of the potent anti-inflammatory drug colchicine in two complementary HF trials.
A trial investigating colchicine in HF due to ischemic heart disease (COLT-HF) is being led by Joseph. By inhibiting common inflammatory pathways that exacerbate HF and atherosclerosis progression, colchicine could reduce HF and ischemic cardiovascular outcomes in patients with HF and IHD. Few HF patients were included in prior colchicine trials of patients with coronary artery disease (CAD) and therefore efficacy and safety needs to be evaluated in this population.
We will conduct a RCT of 2500 participants with HF secondary to IHD and left ventricular ejection fraction less than 0.45, evaluating low dose colchicine versus placebo on the occurrence of the composite HF and ischemic CV outcomes. These complementary trials will evaluate whether targeting inflammation will be beneficial in HF.
Nutritional and environmental exposome
Led by P Raina, Sonia Anand and Salim Yusuf, utilizing our population-based cohort studies and G-CHF registry we will examine how nutrition and the environment (air pollution, climate, social/built environment, and COVID-19) impact HF.

Sonia Anand
We will use food frequency questionnaires (collected in all population-based studies) and more than 1200 nutritional-related metabolomic markers (collected in a subset of 12,000 individuals in PURE) to examine how specific food types, macronutrients, diet quality, and nutritional biomarkers (related to gut microbiome activity, liver/gut metabolism) predict incident HF.
In the G-CHF biomarker sub-study, we will measure levels of these nutritional biomarkers in stored blood samples to examine their relationships with HF outcomes.
In collaboration with environmental epidemiologists, we will also explore how air pollution, variations in temperature, and the social and built environment (e.g. green space, active living friendliness, social deprivation) impact HF. We will also characterize built environment factors important to patients with HF.
In 600 participants in PURE we have collected participant exposures to 1,500 organic or endocrine disrupting environmental chemicals through passive silicone wristband sampling, which can be related to surrogate markers (e.g. N-terminal pro b-type natriuretic peptide) and to incident HF.
We are documenting clinical diagnosis of COVID-19 during follow-up in our cohorts, to examine whether COVID-19 impacts HF development (in PURE and CLSA); and mortality and morbidity in patients HF (in G-CHF).

Darryl Leong
Ageing, comorbidity and HF
Led by PHRI’s Darryl Leong and Guillaume Pare, a team will be serially measuring, in patients in the G-CHF sub-study with stored blood samples, markers of aging (mitochondrial changes, markers of DNA methylation and telomere shortening) which along with frailty, exercise capacity, lung function, echocardiographic parameters, and neuro-hormones to document whether biological markers of aging relate to other physiologic abnormalities and clinical outcomes.
Leong will also lead, with D. Wong, a HF and ageing trial. In patients discharged from hospital with HF, readmissions could be prevented by optimizing self-care behaviors and adherence, but frail patients suffer from geriatric impairments that limit their ability to adopt them.
By assessing geriatric impairments and targeting their treatments using a comprehensive geriatric assessment (CGA), we will test whether this strategy will improve self-efficacy and clinical outcomes. Small studies also suggest that testosterone treatment can improve functional outcomes in older HF patients, but this requires confirmation.
We propose a 2×2 factorial RCT of HF patients older than 65 years with frailty (measured by the Fried index). At hospital discharge, patients will be randomized to a CGA intervention or to usual care. Enrolled males will also be randomized to receive testosterone supplementation or placebo. Outcomes will be death or readmission and health related QOL at one year.
Obesity and HF

Jorge Wong
Obesity results in adverse cardiac (e.g. endothelial dysfunction, fibrosis, pericardial fat restriction) and systemic responses (e.g. plasma volume expansion, high mechanical load, inflammation, RAAS up-regulation) that lead to HF. It is unclear whether weight loss in obese patients prevents HF.
PHRI’s Jorge Wong and Salim Yusuf are leading Bariatric Surgery for Heart Failure Patients (BRAVE), a large RCT testing bariatric surgery (expected to reduce weight by 40 kg on average) versus best medical care in severely obese (BMI >35) participants with CVD (about 500 participants living with HF). Primary outcome will be major CV events, including HF at 5 years. In a subset of 200 individuals, we will test its’ impact on cardiac structure and function by echocardiography. This trial will establish whether weight reduction in obese individuals can reduce HF development or progression.
Improving HF care in the community
Adoption of proven therapies in HF is suboptimal in Canada. Specialized HF clinics improve HF management, but these are mostly located in tertiary hospitals, and accessed by only 10% of HF patients.
There is a lack of integration of care for HF patients in primary care. Building integrated and supported HF care in primary care is crucial to improving HF management in the community, especially in settings where access to a HF clinic is limited. We hypothesize that a NPHW led HF management program delivered in primary care and centrally supported from tertiary care centres will improve HF management and outcomes.
To this end, Heart Outcomes Prevention Evaluation in Heart Failure (HOPE-HF) will be co-led by R McKelvie, Philip Joseph, N Hawkins, and Salim Yusuf. This program will serve as a new model to improve HF management across a range of communities including remote ones in Canada and builds on the successful experiences of HOPE 4 which substantially improved hypertension control in the community (Lancet 2019).
Training, mentoring and capacity development

Eva Lonn
Led by PHRI’s Eva Lonn with J Parker, A Krahn, and J Boulet, the education and training approach will be modelled on the educational model developed by the CDTRP with whom the CHF Alliance has partnered for this purpose. Training and mentoring will occur at all levels through regular virtual training dialogues and multi-day boot-camps (both in-person and virtual), interventions that have proven beneficial by CDTRP to encourage Networking and collaborations between trainees. Priorities include providing trainees with education in research methods such as modern-day epidemiological methods and statistics, pragmatic clinical trials and their implementation, genomics, proteomics, metabolomics, basics of machine learning and AI, cultural and social sensitivities, the involvement of patient partners, health systems, knowledge translation and how policies are developed and implemented, in addition to content knowledge about HF.
As well, foundational competency areas will address communicator, collaborator, manager, health advocate, scholar, and professional roles in the workplace, while the core and individual curricula support competencies in content expertise. Finally, our program of seed funding for early career investigators coupled with mentoring from established investigators, will improve the chances of success of young investigators.
Health disparities, equities, diversity and inclusion

Sonia Anand
Led by PHRIs Michael McGillion and Sonia Anand, with A King and A Krahn, we espouse the Tri-Agency’s commitment to more equitable, diverse, and inclusive Canadian-led research. The composition of our team is guided by the CIHR Gender-Based Analyses Plus (GBA)+ Framework) as well as key principles set forth in the Canada Research Coordinating Committee Progress Report), including interdisciplinary and inclusivity.
We appreciate historical factors and systemic barriers within Canadian society which are replicated and magnified in the Canadian research ecosystem. These impact the scientific career trajectories of women and other underrepresented groups, including (but not limited to): stereotypes that define roles and expectations; lack of role models/mentors; rigid promotional structures; challenges associated with paid work and family life balance; and sexual orientation, ethnicity, and ableism-related prejudices.
The CHF Alliance is comprised of 42% women, 11% Indigenous persons, and 27% identifying as a visible minorities from 29 academic centres in Canada and 5 international, and 8 provinces and 1 territory. We will follow processes and structures that promote equity in Network functioning and participation. Our approach will involve efforts at recruiting and training staff and researchers, emphasizing a culture of inclusion and periodic review and evaluation from an EDI perspective.
Knowledge mobilization

Michael McGillion
Led by Brian Clarke – current president, Canadian Cardiac Transplant network – with A Krahn, M Bains, L West, D Banner, M Bains, and PHRI’s Michael McGillion and Eva Lonn, the network’s KM plan is process-based and consultative with each target population to develop and create content and follow similar processes with partners and across the Network to develop customized approaches. We will integrate the principles of EDI inclusive of Indigenous organizations and underrepresented minorities, and the recruitment of professionals close to underserviced ethnic and demographic groups.
Target Populations for Knowledge and Learning:
- Patients and Families: We will work with HeartLife in creating knowledge relevant to patient needs and priorities, by expanding their strong information platform. Along with the patient-public-partnership cross-cutting team and the CEPPP, our network will identify patient needs for information, and develop mechanisms to make it accessible for patients of various educational and technical sophistication. This will include significant system navigation tools for patients and their families. Additionally, we will assist in mobilizing new knowledge generated by patients and families who actively participate as research partners through the patient-public-partnership cross-cutting team and the CEPPP.
- Health care Professionals: Our network will initiate and lead interventions to optimize interdisciplinary KM to address disparities and variations in care and promote improved patient outcomes. These interventions will be based on the network’s research plan and involve the co-creation of CME programs (i.e., heart failure academy), clinical practice guidelines, and clinical care pathways. Partnerships will include the CCS, the Canadian Heart Failure Society, Canadian Cardiovascular Pharmacists Network, CMA endeavor (primary care), C-Change, and the Canadian Federation of Medical Women.
- General Public: We will develop information/media campaigns for the general public alerting them to risk factors/symptoms of HF so that they may report suspicious symptoms early to their health care provider to reduce the risk of HF and enhance early diagnosis. Network members are involved with the HS Heart Failure Action plan and will work with HS to incorporate their plan into our KM strategy.
- Government and Decision Makers: Integration of decision makers in the development and evaluation of innovations developed by our Network will facilitate translating these into clinical practice and health system policy and influence systems change. We will work with our partners in advocacy efforts to influence systems change at the level of operational decision makers.
- Researchers: We will engage leading researchers, including patient partners, to share findings in high quality journals and other forums. We will work closely with the network training module in the training and education of young clinicians and scientists to improve their skills in this field.
- Industry and technology partners: Many of our discoveries and innovations will be developed and translated in partnership with industry. The Network will engage industry partners as research develops to ensure uptake, further development, and commercialization.

Shrikant Bangdiwala
Data management
Co-led by PHRI’s Shrikant Bangdiwala, with M Harvey, E Jean St Michel, F Dallaire, and S Bedard, we will employ a hub-and-spoke data management model. To the extent possible, data will be held at the Data Management Main Core (DMMC) at the Population Health Research Institute at McMaster University, which will be responsible for the collection, quality assurance, coordination, harmonization, and interoperability, ensuring the integrity and sharing of the Network’s data.
The DMMC will collaborate closely with other data management centres of the Network (e.g. the Hospital for Sick Children and Montreal Heart Institute). Harmonization includes developing and implementing common data dictionaries, common variable definitions, and standardized naming conventions.
In addition to developing guidelines and policies on data sharing in consultation with other members of the Network, the DMMC will take the lead on education and training on data use across the Network, as well as providing helpdesk functions regarding technical data matters.
The training will feature tutorials and demonstrations on various topics from the responsible and ethical use of health-related data for research, Findable, Accessible, Interoperable, and Re-usable (FAIR) health-related data, and statistical considerations in analyses of secondary data from different sources.
Precision health and artificial intelligence
The CHF Alliance has assembled a strong team of precision medicine and AI experts. The CRLB-GMEL (led by Guillaume Pare) and Ted Rogers Centre for Heart Research (S Mital, SickKids) will be the primary laboratories integrating biomarker data from the cohorts. Both groups have substantial expertise in molecular phenotyping using metabolomics, proteomics, transcriptomics and genomics (including rare variant analysis, polygenic risk score development, and Mendelian randomization analyses).
They will be supported by advanced analytic groups through Hamilton Health Sciences (Jeremy Petch, Director, Centre for Data Science and Digital Health – CREATE); SickKids AI in Medicine (M Mazwi, Co-chair), University of Montreal (R Avram, digital health AI and wearables), Laval University & Quebec AI institute (A Durand, reinforcement learning), and MHI (E O’Meara, functional imaging).
These groups bring expertise in multiple domains of machine learning and will employ established and novel AI strategies to improve HF prediction and classification.
Finally, we will collaborate with digital health technology experts in echocardiography (Eko.ai), virtual care and remote monitoring (Michael McGillion, PHRI VICTOR virtual care program), and point of care diagnostics (J Brennan, McMaster Biointerfaces Institute) to identify how these state-of-the-art technologies can best be applied to improve the QOL and clinical course of patients with HF.